3 Ways Hospitals can save money with a clinical-grade Real Time Location System (RTLS)
3 Ways Hospitals can save money with a clinical-grade Real Time Location System (RTLS)
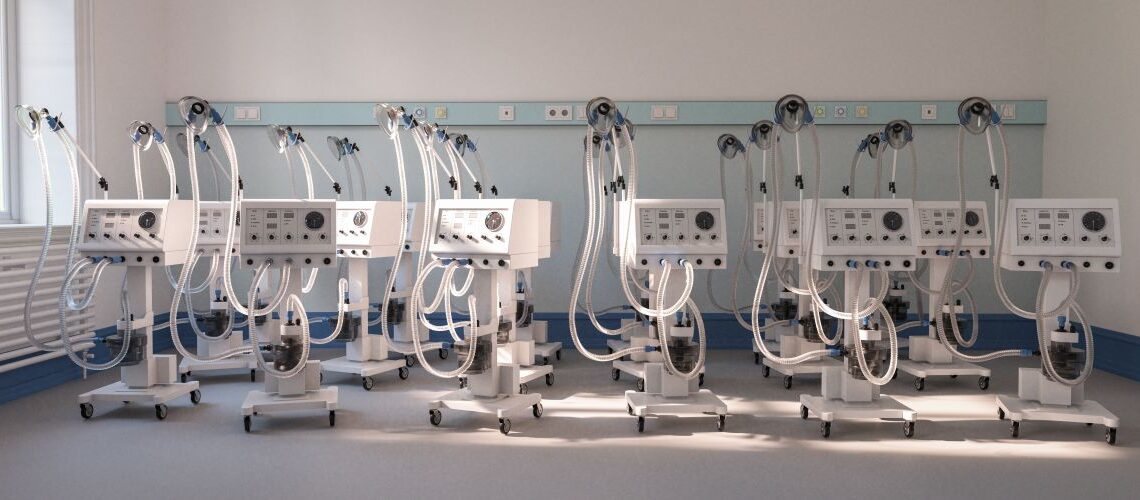
A clinical-grade real time location system (RTLS) like ARINTrack can show you and your staff exactly where to find something (e.g. COVID-19 ventilator) within your hospital thereby improving efficiency and communication throughout the hospital.

1) Find equipment when you need it.
Nurses can spend more time caring for patients instead of searching for equipment.
According to GE Healthcare, nurses spent, on average, 21 minutes per shift looking for equipment- a loss of $500k in non-productive work time. A separate VHA study concurs, finding that nurses spend between 30 minutes and 2.5 hrs. per 12 hour shift searching for equipment.
Frontline care clinicians and staff in hospitals spend at least 10% of their time working around operational failures: situations in which information, supplies, or equipment needed for patient care are insufficient.
The Permanente Journal finds that the cost is significant given that nurses account for approximately one-fourth of a hospital budget.
Seven of the nurses whom we interviewed stated that the equipment needed to do their jobs was often unavailable and that it was accepted practice to “go shopping” in the dirty utility room, in other patients’ rooms, or on other units. For example, one nurse said, “If you can’t find it, you go get it, no matter where it is.
RTLS shows you where your equipment is right now, allowing nurses to find what they need quickly leaving more time to spend on patient care.

2) “Right size” your equipment.
Hospitals can reduce equipment, distribute assets where they are needed most, and show where those available assets can be accessed.
Hospitals have 10-15 medical devices per bed, outfitted uniformly, in the event that any of the devices are needed.
As the number of mobile assets per bed continues to increase, hospitals are stockpiling an enormous amount of underutilized equipment.
Aside from unnecessary rental and purchasing, the cost of unused assets is compounded by routine maintenance fees.
Many hospitals believe, in error, that it is less costly to address equipment availability issues by leasing, renting, or buying more units rather than optimizing how existing devices are managed and distributed. This “redundancy” strategy backfires as the additional equipment simply gets swallowed up in the system, further driving up costs.
According to GE Healthcare, hospitals own 35,000 inventory SKUs and utilization hovers around 32-38%. Nationwide, hospitals are overspending billions each year — usually unknowingly— on mobile assets that are not utilized effectively.
According to our calculations, the average 200-bed hospital could avoid $1.3 million in capital expenditures and reduce annual service costs by $160,000 simply by reducing its inventory of mobile devices by 25 percent—a reasonable and achievable goal.
Unused equipment has an associated cost, does not make money, and can be removed. RTLS can show you when and where your equipment is being used and when it is not used.

3) Decrease bed turnover times. Increase throughput.
Improve interconnectedness between departments and reduce operational failures. RTLS shows the location and, potentially, status of room assets to all departments across the organization.
Reducing room turnover time is important for hospitals because it can increase bed utilization, which lowers the hospital’s cost structure. It also enables incoming patients to begin treatment sooner, which improves patient care and reduces length of stay. We consider a room to be ready when it has been properly cleaned; it has the appropriate bed, equipment, and supplies needed by the patient; and the nurse is mentally ready to provide care.
A study by The Permanente Journal identified internal supply chain as the primary source of operational failure for room turnover. Nursing units had the highest number of items as budgetary responsibility, but the responsibility for supplying, cleaning, and maintaining the items fell to other departments. BMC Emergency Medicine quantifies the cascading effect of added inpatient time at nearly $1000 per day.
The cumulative effect of delay on the 1558 patients who experienced delay was an additional 2,183 hospital days and $2,109,173 in incremental cost.
In an organization where department performance is rewarded, overall hospital performance can suffer. A hospital wide RTLS enables optimization of processes across departments through examination of equipment and material flow.
Conclusion
Implementing a RTLS system like ARINTrack can improve operational efficiency by allowing nurses to do what they do best – spending more time on patient care. Cut costs by reducing the amount of extra equipment needed and the time required for bed turnover.